HEALTH
How Clinical Trials Are Making Personalized Medicine Possible
Introduction to Personalized Medicine
Personalized medicine is an evolving field that customizes healthcare to the distinct biological and lifestyle factors of each individual. By leveraging insights from a patient’s genetic makeup, environment, and daily habits, personalized medicine seeks to provide treatments that are more effective and less likely to cause unwanted side effects than conventional approaches. This innovative model stands in contrast to the traditional, generalized treatment plans that have dominated medicine for decades, wherein patients with the same diagnosis often received similar interventions regardless of their unique differences. Early engagement with clinical research not only helps establish safe and precise therapies but also empowers individuals looking to find a clinical trial suited to their unique health profile, encouraging a more proactive and informed approach to personal health.
As the demand for tailored healthcare escalates, the medical community is doubling down on technologies and methods that prioritize individual differences. With advancements in genomics, data analytics, and digital health, the personalization of care is quickly transforming both prevention and treatment strategies. These tools enable a deeper exploration of what makes each person’s health status unique, allowing for the identification of genetic variants, biomarker patterns, and other characteristics that can significantly influence disease risk, drug response, and overall prognosis. This shift is enhancing standards of care by identifying treatment pathways that yield better outcomes for distinct subgroups of patients within large, diverse populations. Ultimately, this trend is moving medicine closer to the ideal of providing the right treatment, to the right person, at the right time.
The Role of Clinical Trials in Personalized Medicine
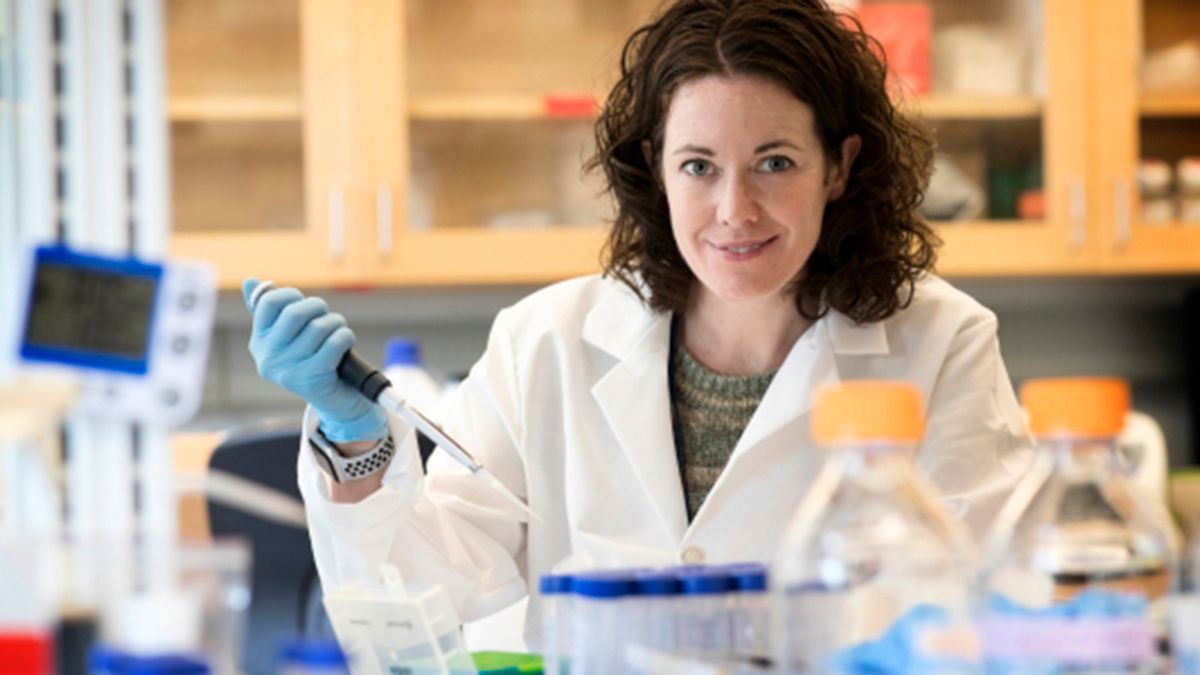
Clinical trials are fundamental in unlocking the full potential of personalized medicine. These trials act as testbeds for evaluating the safety and effectiveness of new therapies in specific patient groups, often stratified by genetic profile, age, gender, or lifestyle. By collecting and analyzing outcomes from diverse cohorts, researchers can identify which interventions are most effective for specific individuals and understand why. This data-driven approach is vital in ensuring that tailored treatments not only work in theory but also deliver real-world benefits, such as improved survival, reduced adverse events, and an overall better quality of life for patients.
Data from these trials not only helps healthcare providers make informed treatment recommendations but also supports regulatory agencies in their approval process. Insights gained from meticulously designed trials guide doctors in matching interventions to each patient’s needs while confirming efficacy and safety on a population level. As more targeted therapies transition from experimental to mainstream, patient participation is enabling a richer understanding of how diseases behave, evolve, and respond to various interventions. For those actively seeking tailored healthcare solutions, participating in a clinical investigation accelerates progress while offering access to advanced treatments that may otherwise not be available through standard care.
Advancements in Clinical Trial Design
The growing sophistication of clinical trial protocols is paving the way for the next generation of personalized therapies. Among recent breakthroughs are adaptive trial designs, which allow for mid-study modifications to optimize resources and outcomes. In adaptive trials, researchers can alter key elements—such as dosing, sample size, or even study endpoints—based on interim results, all without compromising the scientific rigor or validity of the trial. This flexibility in trial methodology ensures that ineffective treatments can be quickly set aside, while promising interventions receive greater focus. These innovations streamline the path to identifying optimal regimens for specific patient populations, thereby accelerating the discovery of promising therapies and reducing both the time and costs associated with bringing new drugs to market.
Adaptive clinical trials facilitate continuous learning and adjustment, a critical advantage when treating heterogeneous diseases like cancer or rare genetic disorders. Traditional trial designs often struggle with these conditions because of their variability, but adaptive designs can rapidly cycle through different therapeutic options guided by real-time data. This approach enables scientists and clinicians to more efficiently identify the most beneficial therapies for subgroups that were previously overlooked in traditional trials. The ability to adjust protocols mid-course allows researchers to maximize both efficiency and patient benefit, a significant step forward in the era of precision medicine.
Artificial Intelligence Enhancing Clinical Trials
Artificial intelligence (AI) has emerged as a game-changer in clinical research, providing powerful tools to accelerate trials, make them more predictive, and increasingly individualized. Machine learning models can sift through enormous volumes of health records, identifying patients most likely to benefit from a new drug or therapy. This vast and rapid analysis not only saves time but also increases the accuracy with which patients are selected for trials, enhancing both the efficiency and reliability of research outcomes. These insights significantly enhance patient recruitment, stratification, and monitoring, ultimately yielding results that are more relevant to precision medicine.
Applications of AI extend to predicting disease progression and response to treatment, especially in complex conditions such as cancer or rare metabolic disorders. For example, AI-driven platforms have already demonstrated their ability to anticipate how tumors will evolve based on molecular profiles, paving the way for adaptive, patient-specific care strategies. Tools leveraging deep learning and predictive analytics help doctors chart a more precise course of therapy, which is substantially more likely to achieve the desired outcomes for each patient. The New York Times discusses how AI is transforming medicine, including its increasing impact on clinical research and its potential to revolutionize the conduct, interpretation, and application of trials in everyday clinical practice.
Real-World Applications of Personalized Clinical Trials
Clinical trials informed by principles of personalized medicine have yielded measurable success stories in recent years. For instance, a groundbreaking study at the University of California, San Diego showcased how customizing cancer therapies to match the genetic profile of each patient’s tumor significantly improved survival outcomes and reduced unnecessary side effects. This research found that individuals receiving treatments tailored to the genetic alterations driving their cancer benefited from a more targeted attack against cancer cells, while being spared from exposure to irrelevant or potentially toxic therapies. These results underscore the ability of personalized clinical trials to deliver therapies that are as unique as the individuals they target, fundamentally changing patient expectations and standards of care.
Similarly, precision treatments are now extending beyond oncology to fields such as cardiology, neurology, and rare diseases. In heart disease, for example, researchers can identify genetic markers that predict how a patient will respond to blood thinners, cholesterol-lowering medications, or antiarrhythmic agents, thereby reducing dangerous side effects and improving treatment success rates. In neurology, clinical trials for Alzheimer’s and epilepsy now often consider specific genetic variants and biomarkers, leading to earlier and more effective interventions. In these disciplines, integrating genetic and real-world patient data has accelerated the development of targeted therapies, enhancing both the quality of life and prognosis for conditions that previously had limited treatment options. Evidence continues to mount that the tailored approach of personalized clinical trials offers real promise for the future of medicine and for millions of patients with complex, previously untreatable diseases.
Challenges in Implementing Personalized Clinical Trials
Despite significant progress, multiple hurdles remain before personalized clinical trials can become standard practice. One major obstacle is gathering and validating high-quality data across diverse patient populations to refine predictive models, as the underrepresentation of certain groups can skew results. There are also challenges in aligning medical infrastructure and data systems to handle this volume and complexity of data while preserving patient privacy and meeting strict regulatory requirements. Ensuring equitable access to trial participation and advanced treatments also remains a challenge, with disparities often driven by geographic, socioeconomic, or systemic barriers. Bridging these gaps is essential to prevent the benefits of personalized medicine from being limited to select subgroups while others are left behind.
Integrating personalized trial results into routine clinical practice requires updated infrastructure, continuous medical education, and collaboration across disciplines. Physicians, nurses, and other providers must stay informed on emerging therapies and approved indications, while also being equipped to communicate complex genomic information to patients. As the regulatory environment continually evolves, frameworks are needed to protect patient privacy while facilitating ethical and transparent data sharing between researchers, clinicians, and patients. Industry standards need to keep pace with innovation to ensure safety, accountability, and trust in new precision therapies, ultimately shaping a sustainable future for personalized research and care.
The Future of Personalized Medicine Through Clinical Trials
With ongoing advances in data science, genomics, and trial methodology, personalized medicine is poised for exponential growth. Comprehensive collaboration among academic institutions, technology companies, healthcare providers, and regulatory agencies will be crucial to dismantling the remaining obstacles and bringing the full possibilities of individualized therapy within reach for more patients. With increasingly refined tools to dissect disease at the molecular level, clinical researchers are poised to generate actionable insights in less time and with greater accuracy, making previously unimaginable breakthroughs closer to reality. The potential for even more individualized and effective treatment modalities is vast, with personalized clinical trials catalyzing practical, evidence-based change and charting the course for medicine in the coming decades.
As the frontier of healthcare continues to move toward personalization, clinical trials will remain at the center—testing, validating, and refining the therapies of tomorrow. These efforts hold the promise not just for improved treatments but for a fundamental reimagining of how diseases are understood and managed. By embracing these advances, healthcare systems and providers can establish a more adaptable, patient-centered framework where individuals receive tailored care that evolves in line with the latest scientific understanding.
Final Thoughts
Clinical trials provide the foundation for making personalized medicine a reality, transforming hopeful concepts into proven therapies tailored for each person. Through ongoing innovation in trial design, the integration of AI, and the accumulation of real-world data, clinical trials are establishing a new standard of individualized care. By participating in or supporting clinical research, patients and providers alike can help accelerate the arrival of a future where every patient receives the right treatment at the right time. With these collective efforts, the vision of medicine that is informed, intentional, and personal can be realized—improving outcomes and redefining healthcare for generations to come.
HEALTH
The Comprehensive Benefits and Future Potential of Telehealth Therapy in Modern Mental Health Care

Introduction
Mental health has become a central focus of contemporary healthcare, yet many individuals face barriers that prevent them from seeking traditional in-person therapy. Factors such as time constraints, mobility issues, and social stigma often make it challenging for people to access consistent mental health support. In this context, telehealth therapy has emerged as a transformative solution, providing effective and flexible treatment options that can reach a wide range of individuals without compromising quality.
Telehealth therapy leverages digital technology to connect clients with licensed mental health professionals remotely. By integrating communication platforms, virtual tools, and secure data-sharing systems, it allows individuals to receive therapy in ways that were previously impossible. This approach not only makes mental health care more accessible but also enables innovative methods of monitoring, support, and intervention.
Understanding Telehealth Therapy
Telehealth therapy is a form of mental health care delivered through digital channels such as video conferencing, phone consultations, or secure messaging apps. It mirrors traditional therapy in its core principles while providing the convenience of remote access. Patients can participate in sessions from their homes, offices, or other private spaces, which helps eliminate barriers related to transportation, scheduling, or physical accessibility.
The process of telehealth therapy is designed to be user-friendly and secure. Therapists use encrypted platforms to conduct sessions, ensuring confidentiality while maintaining therapeutic efficacy. The range of services available is extensive, including cognitive-behavioral therapy (CBT), psychodynamic therapy, group counseling, and family therapy. Virtual therapy sessions can also incorporate digital tools, progress tracking, and supplementary exercises to enhance treatment outcomes.
Advantages of Telehealth Therapy
One of the most significant benefits of telehealth therapy is enhanced accessibility. By removing physical and logistical barriers, individuals who might not otherwise seek therapy can access professional mental health support. This is particularly important for those with mobility limitations, busy schedules, or social anxiety that makes in-person interactions difficult.
Convenience is another key advantage. Telehealth therapy sessions can be scheduled flexibly, often outside of standard business hours, which encourages consistency in treatment. Patients no longer need to worry about commuting, childcare, or time away from work, making it easier to maintain regular sessions.
Privacy and discretion are also crucial benefits. Many individuals hesitate to seek traditional therapy due to fear of stigma or unwanted attention. Telehealth therapy provides a private environment where patients can engage openly and honestly, fostering a sense of safety and comfort.
Additionally, telehealth therapy supports continuity of care. Patients who travel frequently, experience life transitions, or face health limitations can maintain ongoing relationships with their therapists without disruption. This uninterrupted access to care improves treatment adherence and long-term outcomes.
Evidence-Based Effectiveness
Numerous studies demonstrate that telehealth therapy can be as effective as traditional in-person sessions for a variety of mental health conditions. Research shows that conditions such as depression, anxiety, post-traumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD) respond well to virtual interventions. Patients often report similar levels of symptom improvement, treatment satisfaction, and adherence to therapeutic recommendations compared to conventional therapy.
Telehealth therapy also enables innovative data collection and monitoring. Many platforms allow therapists to track clients’ progress through digital tools, logging mood patterns, sleep habits, or behavioral triggers. This data-driven approach enables therapists to personalize treatment plans, detect potential challenges early, and provide targeted support, improving overall effectiveness.
Approaches and Techniques Used in Telehealth Therapy
Telehealth therapy can accommodate a wide range of therapeutic approaches, making it versatile for different needs and preferences. Cognitive-behavioral therapy (CBT) is particularly well-suited for virtual delivery. Therapists can guide clients through structured exercises, homework assignments, and thought-restructuring activities, all within a secure digital environment.
Other common approaches include psychodynamic therapy, interpersonal therapy, family therapy, and group sessions. Specialized treatments, such as dialectical behavior therapy (DBT) for emotional regulation or exposure therapy for phobias, can also be adapted for online sessions. Tools like video demonstrations, interactive exercises, and secure messaging enhance the therapeutic experience and ensure engagement.
Telehealth therapy often incorporates supplementary resources such as mindfulness exercises, guided journaling prompts, and educational modules. These resources complement live sessions, encouraging active participation in therapy and empowering patients to take ownership of their mental health journey.
Challenges and Considerations
Despite its numerous advantages, telehealth therapy is not without challenges. Technology barriers can limit accessibility for some individuals. Reliable internet access, compatible devices, and digital literacy are all necessary to participate effectively in virtual therapy.
Maintaining privacy and security is another critical consideration. Telehealth therapy relies on secure platforms with encryption to protect sensitive client information. Therapists must adhere to strict confidentiality standards to ensure trust and compliance with ethical guidelines.
Insurance coverage can also pose limitations. While many providers now cover virtual therapy sessions, policies vary, and some patients may face financial barriers. Awareness of coverage options is essential for both patients and therapists to navigate these challenges effectively.
Additionally, some patients may find virtual interactions less personal than in-person sessions. Non-verbal cues, subtle emotional signals, and physical presence play an important role in building rapport. Therapists must employ specialized techniques to foster connection and engagement in a digital environment.
The Future of Telehealth Therapy
The potential of telehealth therapy continues to expand as technology evolves. Artificial intelligence (AI) and machine learning are beginning to enhance therapy by analyzing speech patterns, mood changes, and behavioral indicators to provide insights for therapists. Virtual reality (VR) and augmented reality (AR) are emerging as tools for immersive treatment, particularly in exposure therapy and skill-building exercises.
Integration with wearable devices can further support telehealth therapy by tracking physiological indicators such as sleep patterns, heart rate, and stress levels. This real-time data allows therapists to proactively adjust treatment plans, offer targeted interventions, and improve overall care quality.
As telehealth therapy becomes more sophisticated, it is likely to play an increasingly central role in modern mental health care. Its combination of accessibility, flexibility, and effectiveness positions it as a critical solution for addressing growing mental health needs.
Conclusion
Telehealth therapy has revolutionized the way mental health care is delivered. By breaking down barriers to access, providing convenience, and offering evidence-based effectiveness, it has created new opportunities for individuals seeking mental health support. While challenges related to technology, privacy, and insurance remain, ongoing innovations continue to enhance the effectiveness and reach of virtual therapy.
As the demand for mental health services grows, telehealth therapy stands out as a vital component of modern care. It empowers individuals to prioritize their mental well-being while giving therapists new tools to provide flexible, personalized, and high-quality support. The continued integration of technology in mental health care signals a promising future, where therapy is more accessible, efficient, and impactful than ever before.
HEALTH
Common Dog Issues That CBD Treats May Help With

Dogs can experience stress, pain, or health concerns at different stages of life. Some may feel anxious when left alone or develop stiffness as they age. Others may have digestive or skin-related troubles that affect their comfort. These issues can impact their mood, sleep, and behavior if not managed properly.
That’s why many pet owners are exploring natural ways to support their dogs’ wellness. CBD Dog Treats are one such option that may help ease anxiety, support mobility, and promote balance in the body. When used under a vet’s guidance, they can complement other care routines and make your pup’s life calmer and happier.
Ease Anxiety and Stress
Many dogs experience anxiety during car rides, loud weather, or periods of separation. They may bark excessively, pace, or hide. CBD helps calm the body’s stress responses and promotes a sense of ease without dulling alertness.
By using natural calming compounds, these treats can reduce nervous tension and help them settle more quickly. Pairing them with gentle reassurance and predictable routines strengthens the sense of safety they feel at home. Over time, dogs may show more relaxed behavior even in situations that once caused distress.
Support Joint and Mobility Health
Joint stiffness can limit how dogs move and play. Age, injury, or excess weight can put pressure on joints, leading to pain and fatigue. CBD has anti-inflammatory properties that may help reduce swelling and discomfort, making movement smoother.
When dogs can walk or climb stairs without pain, their mood and energy rise noticeably. Combine regular CBD treats with a balanced diet and moderate exercise for better joint strength over time. This approach helps preserve long-term mobility and supports a more active lifestyle.
Promote Digestive Balance
Digestive distress can appear in several ways, including irregular appetite, bloating, or gas. CBD supports the body’s internal systems by calming irritation in the gut and improving comfort. It may also help regulate appetite and reduce nausea in sensitive dogs.
Healthy digestion means your pet absorbs nutrients more effectively. That leads to stronger immunity, better coat condition, and higher daily energy levels. Maintaining a steady feeding schedule alongside CBD support further improves your pet’s gut health.
Skin Irritation and Allergies
Itching, redness, and dry patches can make dogs restless and uncomfortable. These signs may point to allergies caused by diet, environment, or fleas. CBD’s natural calming effects can help reduce inflammation and relieve skin irritation over time.
Adding CBD Dog Treats to your pet’s daily care may support healthy skin and coat texture. Along with regular grooming and a balanced diet, this routine helps restore moisture and comfort, keeping your pup at ease throughout the year. Continued care prevents flare-ups and promotes lasting relief for sensitive pets.
Manage Age-Related Discomfort
Senior dogs deserve extra care as their bodies change. Aging can bring slower movement, stiff joints, and disrupted sleep. CBD can help relieve minor aches, soothe discomfort, and promote better rest for older pets.
A calm, well-rested dog is more likely to stay social and active. Combined with vet supervision and gentle exercise, CBD supports a happier and more mobile life for senior companions. A consistent wellness routine can greatly improve their quality of life as they age.
Dogs experience many physical and emotional challenges as they grow. Issues such as anxiety, poor digestion, and skin irritation can reduce their comfort and quality of life. Natural aids like CBD Dog Treats can help restore balance and provide gentle relief when used responsibly. With consistent care, the right diet, and regular vet visits, your pet can stay healthier, calmer, and full of vitality every day.
HEALTH
How to Thrive as a Modern Caregiver

Caregiving today is an intricate blend of empathy, resilience, and skill, requiring much more than a simple willingness to help. The role of a caregiver extends beyond the basics of physical care; it demands deep understanding, adaptability, and ongoing commitment. For those who care for loved ones or work professionally as caregivers, the daily and long-term demands can be immense, but so too can the deeply meaningful rewards. Balancing compassionate, effective support with attention to your own well-being is essential for sustaining the energy and mindset needed to provide excellent care over time. By exploring new opportunities, resources, and support networks, caregivers can ensure their journey is less isolating and far more sustainable. See job postings to explore caregiving opportunities and connect with a larger, supportive community that understands your unique challenges and values all that you contribute.
Modern caregivers face evolving challenges that require a flexible mindset. From managing multiple medications and healthcare appointments to shouldering the emotional labor of supporting a loved one, or juggling professional responsibilities alongside personal caregiving, every day may bring something new. Embracing the wide range of resources available, tapping into innovative technologies, and building strong support systems can make a remarkable difference in both daily effectiveness and long-term satisfaction. Whether you’re brand new to caregiving, have years of experience, or are looking to enhance your approach, developing practical skills and understanding tried-and-true strategies will help you truly thrive while supporting others in need.
Prioritize Self-Care
The foundation of effective caregiving lies in the caregiver’s own health and resilience. Physical self-care involves more than just ticking boxes—it means being attentive to your body’s cues for rest, engaging in regular exercise, eating nutritious meals, and prioritizing adequate sleep. These seemingly simple habits power your ability to respond with patience, energy, and competence in your caregiving role, even during high-stress periods. Emotional self-care is equally vital and too often overlooked; small practices like daily meditation, expressing yourself through creative hobbies, or simply finding moments of quiet reflection can help you process emotions and maintain your sense of purpose and joy.
Making room in your routine, whether daily or weekly, for restorative “me time” isn’t selfish; it’s necessary. Research shows that when caregivers neglect their own needs, risks of stress, fatigue, depression, and even medical errors soar. Intentionally investing in yourself by scheduling self-care activities and honoring those commitments lets you give your best throughout every challenge and change. A refreshed and centered caregiver is far more capable of delivering attentive, compassionate care to others, making self-care a non-negotiable part of sustainable caregiving.
Establish a Strong Support System
No caregiver is meant to navigate the journey alone. Establishing a robust, reliable network of support is fundamental for lightening the burden, reducing stress, and gaining a meaningful perspective. Lean on your existing support system, family, friends, neighbors, or consider reaching out to professionals such as care coordinators, counselors, or home healthcare aides for extra assistance. Don’t hesitate to connect with online caregiver communities or attend local support groups, which offer empathetic spaces to share advice, celebrate small victories, and find camaraderie during tough times. Simply knowing you’re not alone, and having somewhere to turn, can transform even the most difficult moments into manageable ones. Remember, asking for help is a sign of strength, not weakness, and can empower you to be a more effective and fulfilled caregiver.
Stay Organized with Daily Routines
Time management is one of the cornerstones of thriving as a modern caregiver. Building predictable daily routines and sticking to them as much as possible helps bring order, structure, and greater peace of mind to everyone involved. Begin by setting up clear to-do lists each morning or week. This not only helps prioritize the most important tasks but also provides a sense of accomplishment as items get completed. Digital planners or specialized caregiving apps can efficiently and securely track medications, appointments, and other vital responsibilities, which is especially helpful as demands become more complex. Whenever possible, don’t be afraid to delegate appropriate tasks to others, such as relatives, friends, or community volunteers; this lightens your load and allows you to focus on higher-priority care. Well-designed routines, paired with teamwork, create a sense of shared responsibility, reduce oversights, and make adjusting to new challenges less overwhelming.
Expand Your Knowledge and Skills
The world of caregiving is always evolving, presenting new information, challenges, and opportunities for personal and professional growth. Staying informed and seeking ongoing education are among the most effective ways to enhance the quality of support you provide. Whether you’re caring for someone with a chronic illness, dementia, or disabilities, different scenarios benefit from specialized skills and up-to-date techniques. Numerous online courses, webinars, and in-person workshops, offered by trusted organizations and healthcare providers, cover essential topics such as safety, first aid, behavioral management, and effective communication.
Seeking formal certification, such as becoming a Certified Nursing Assistant (CNA) or pursuing specific credentials in dementia care, not only deepens your expertise but can also open doors to new career opportunities or higher compensation, if you’re a professional caregiver. Embracing new caregiving technologies, like digital medication organizers and telehealth services, can simplify daily routines and empower caregivers with timely reminders, alerts, and real-time professional guidance.
Manage Stress and Prevent Burnout
Unchecked stress is one of the most significant risks caregivers face and can quickly lead to burnout, which undermines not just your well-being but also the quality of care you give. Establishing daily or weekly opportunities for self-renewal is key to long-term resilience—this could include anything from brief walks outdoors and listening to relaxing music, to practicing deep breathing or mindfulness techniques. Regular, scheduled breaks—even just 10–15 minutes—act as powerful safeguards against exhaustion and help you return to your caregiving role with a clearer mind and a lighter spirit.
If you ever find yourself dealing with ongoing sadness, anxiety, or feelings of hopelessness, it’s crucial to seek out professional guidance promptly. Counseling or therapy is a proactive, healthy step for any caregiver facing emotional strain and can be a game-changer for regaining perspective and strength.
Embrace Technological Innovations
Technology is rapidly transforming the caregiving experience, often in ways that promote safety, efficiency, and peace of mind. Innovative smartphone applications, wearable health monitors, and smart home systems offer unprecedented convenience, making it easier than ever to stay organized and connected, even from a distance. Medication adherence platforms like Adhera, for example, provide automated reminders and real-time feedback, increasing accuracy and boosting both caregiver and patient confidence. These advances streamline routines, reduce errors, and keep caregivers informed, leading to improved daily outcomes and overall quality of life for everyone involved.
Advocate for Caregiver-Friendly Workplaces
Many caregivers also hold demanding professional jobs, making balancing these dual responsibilities particularly challenging. Advocating for caregiver-friendly policies in your workplace, such as flexible schedules, remote work options, or formal caregiver support programs, can make a world of difference for both your career and your sense of well-being. Forward-thinking employers are increasingly recognizing the value of accommodating caregivers, which, in turn, boosts employee morale, productivity, and retention.
Final Thoughts
Modern caregiving is both complex and rewarding, and with the right foundation, caregivers can truly thrive. Integrating self-care, cultivating strong support networks, maintaining organization, pursuing ongoing growth, managing stress, embracing technology, and advocating for workplace flexibility are all vital components of resilience and effectiveness. These practices support not only the caregiver’s well-being but also ensure those in their care receive the highest possible quality of attention and support. Always remember: your well-being is every bit as important as those you support. By investing in yourself and embracing a balanced approach, you set the stage for sustained, high-quality caregiving through every season and challenge that life may bring.
-

 TOPIC6 months ago
TOPIC6 months agoSymbols of Hope: The 15th Belenismo sa Tarlac
-

 TOPIC6 months ago
TOPIC6 months ago“The Journey Beyond Fashion” – Ditta Sandico
-

 NEWS6 months ago
NEWS6 months agoHistorical Churches in Manila
-
 TOPIC6 months ago
TOPIC6 months agoRIZAL at 160: a Filipino Feat in Britain
-

 TOPIC6 months ago
TOPIC6 months agoBoats with Two Strings
-

 TOPIC6 months ago
TOPIC6 months ago5 Must-Have Products From Adarna House to Nurture Your Roots
-

 TOPIC6 months ago
TOPIC6 months ago“Recuerdos de Filipinas – Felix Laureano”
-

 TOPIC4 weeks ago
TOPIC4 weeks agoUnveiling AvTub: Your Ultimate Guide to the Best AV Content
